Medical Billing Automation
BLOG
7 min read
How to Build an Automated Medical Billing System and Why You Need It
Billing and payment procedures in the healthcare industry can be difficult and exhausting. It typically requires a lot of manual labor, such as filling out paperwork and double-checking data to make sure everything is accurate and complies with laws. This procedure can be mistake-prone and is frequently slow.
This is made easier by an automated medical billing system, which uses technology to complete these chores more quickly. The system uses software to handle data entry and claim processing automatically, saving human labor. As a result, claims are handled more quickly, errors are decreased, and payments are managed more precisely.
These systems integrate several tasks, into a single, efficient tool, such as tracking payments, coding medical services, confirming insurance, and setting up appointments. By doing this, healthcare providers can save time, reduce mistakes, and concentrate more on patient care than on paperwork.
In this blog, we will explore how to build an automated medical billing system and why you should do it.
Want to reduce billing errors and speed up payments?
Let’s Automate!What Is Medical Billing Automation?
For healthcare providers, medical bills can be a major source of stress. It's labor-intensive, intricate, and prone to mistakes. Imagine having to follow down payments, enter data manually, and stay on top of ever changing insurance regulations. Ouch!
The good news is that automation for medical billing can save the day for you! It can take care of all the tedious, monotonous work so you can deliver top-notch patient care. So, how does this work? Medical billing automation automates operations such as coding, payments, and compliance with financial forms by using tools and intelligent software. This translates to fewer errors, quicker processing, and enhanced cash flow.
Why Automate Medical Billing?
Automated medical billing is more than a trend, it is rather turning into a requirement for healthcare providers who want to modernize their outdated systems and optimize their operations. The following are some benefits of medical billing automation.
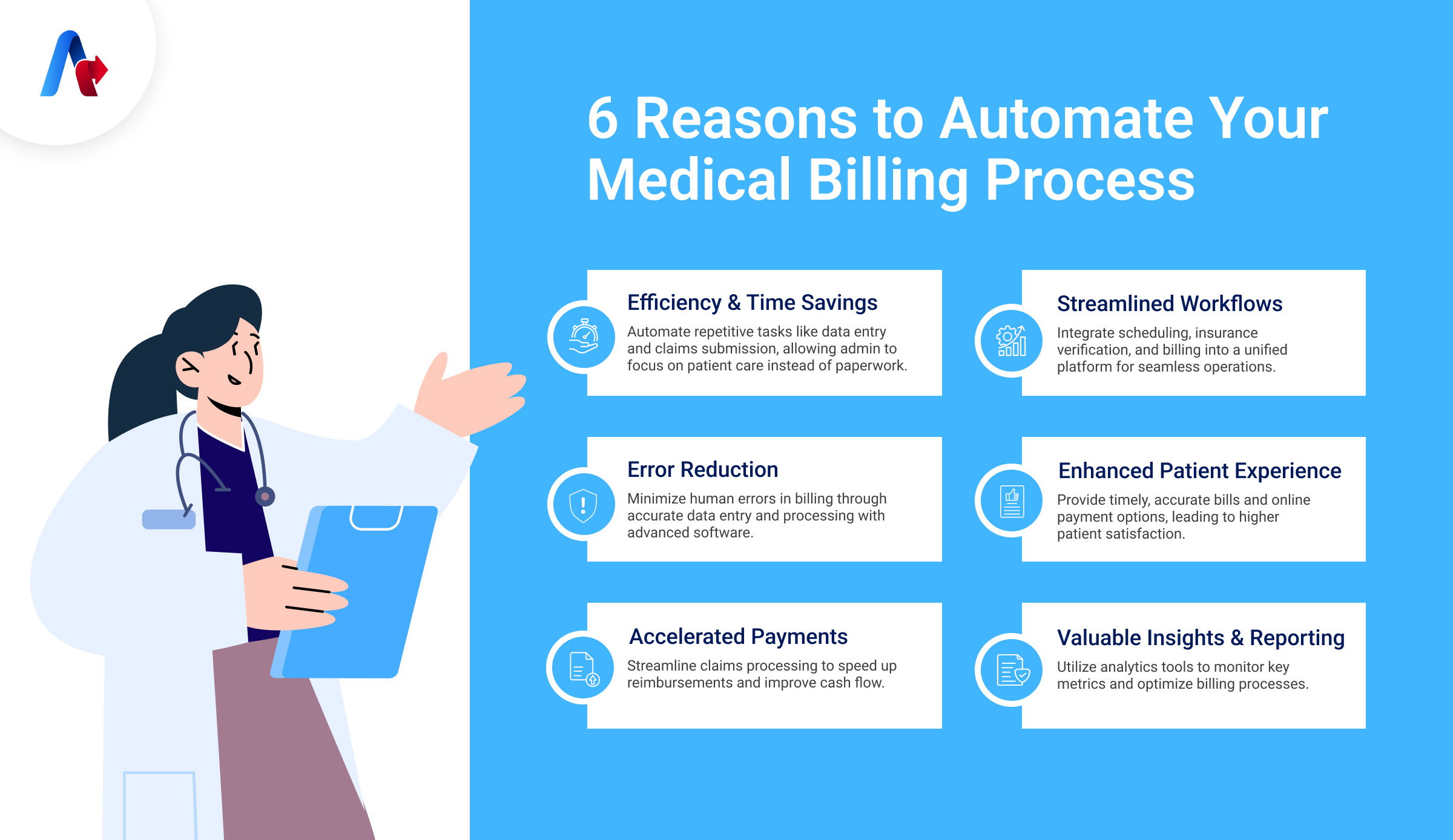
1. Effectiveness and Time Savings
By automating repetitive operations, automated medical billing systems transform the way medical billing process is managed. This means that tasks like data entry, claim submission, and payment tracking are automated. As a result, your administrative team won't have to spend as much time and effort on paperwork and more time caring for patients. For example, the technology processes hundreds of claims in minutes as opposed to hundreds of claims being processed manually every month.
2. Error Mitigation
Human error can occur when billing manually, such as when patient data is entered incorrectly, or insurance codes are misinterpreted. Medical billing automation reduces these errors by using the advanced software to precisely manage data input and processing activities. Here, Robotic Process Automation for medical billing (RPA for medical billing) is essential since it automates repetitive, rule-based processes, guaranteeing the accuracy of patient data and billing codes.
3. Quick Payments
Faster reimbursement is one of the main advantages of healthcare payment automation. The whole claims process—from filing to follow-up—is streamlined by automated systems. This expedites the process of approving claims and disbursing compensation. Automated billing systems can detect and resolve problems that could cause delayed payments, improving your cash flow and reducing the time you spend on collections.
4. Simplified Procedures
Automated health management systems provide a single, integrated platform that combines multiple tasks into one, such as insurance verification, invoicing, and scheduling. With all the parts of the billing process connected and information flowing easily from one activity to the next, this integration aids in the creation of a smooth workflow. This means reduction in manual handoffs and an improved method of handling patient data and invoicing duties.
5. Improved Healthcare Experience for Patients
Patients gain from a more efficient and clear billing experience that is possible from automated billing services and automated healthcare payments. Automated systems have the ability to issue bills on time and accurately, give online payment choices, and clearly explain charges. In addition to decreasing billing conflicts, this also increases patient satisfaction by simplifying things for patients to grasp.
6. Valuable Insights and Reports
Automated systems include analytics and reporting capabilities that offer insightful information about your invoicing processes. You can keep an eye on important indicators like claim acceptance rates, payment turnaround times, and outstanding balances by examining these reports. You may use this data to better your billing operations by identifying trends, identifying possible problems, and making well-informed decisions.
Need a smarter way to manage healthcare operations?
Talk to Our Experts Today!How to Implement RPA in Medical Billing?
Building an automated medical billing system requires strategic planning, expert guidance and the right tools. Here is a simple step-by-step approach that you can follow to successfully implement RPA for medical billing.

1. Identify Automation Opportunities
- Data Extraction: Automate the retrieval of patient information from Electronic Health Records (EHR), reducing manual data entry and improving data accuracy.
- Claim Creation: Use automation to populate claim forms with accurate data and apply appropriate coding, ensuring consistency and reducing the risk of errors.
- Claim Submission: Automate the submission of claims to insurance providers, managing electronic remittance and reducing the time spent on manual submissions.
- Status Tracking: Implement automated tracking of claim statuses, handling rejections, denials, and follow-ups efficiently to expedite the resolution process.
2. Design and Develop RPA Bots
- Data Extraction Bot: Extracts patient data from EHR systems, cleanses it, and prepares it for billing, improving data accuracy and consistency.
- Claim Creation Bot: Automates the process of entering data into billing systems, generating claims, and ensuring accurate coding and compliance with billing regulations.
- Claim Submission Bot: Handles electronic submission of claims to insurance providers and manages confirmation receipts, streamlining the claims process.
- Status Tracking Bot: Monitors the status of claims, identifies issues, and triggers follow-up actions or adjustments as needed, enhancing the management of claims and payments.
3. Test and Deploy
- Pilot Testing: Conduct thorough testing with sample data to ensure that the bot’s function correctly and integrate seamlessly with existing systems. Address any issues identified during testing to refine the automation process before full deployment.
- Deployment: Roll out the automation solution across the billing process, providing training to staff as needed and monitoring the system’s performance to ensure it meets the desired outcomes.
4. Continuous Improvement
- Feedback and Optimization: Regularly collect feedback from users and monitor the performance of the RPA system. Use this information to make continuous improvements, address any issues, and refine processes for even greater efficiency and accuracy.
Automation not only transforms billing processes but also supports the broader goal of improving overall healthcare delivery and management.
Automated Solutions to Simplify Medical Billing
For healthcare firms, automating their medical billing procedures can be an innovative approach. Why? By using automated medical billing systems, you can reduce errors, speed up payments, and streamline workflows, enabling you to focus more on patient care. Partnering with a trusted global automation service provider like Accelirate can help you effectively to implement medical billing automation with ease and precision.