Revenue Cycle Management Automation
BLOG
8 min read
How AI Agents-Powered RPA Is Optimizing Revenue Cycle Management in Healthcare
Managing revenue cycles efficiently is essential for healthcare providers. Revenue Cycle Management (RCM) includes all the administrative and clinical processes needed to track patient interactions, from registration to final payment. However, many RCM tasks rely on manual efforts, leading to errors, delays, and increased costs. Robotic Process Automation (RPA) powered by intelligent agents is changing this by working autonomously to automate repetitive tasks, improve accuracy, and make processes more efficient.
How much time does your team spend on manual RCM tasks each day?
Tell Us!What is RCM Automation with Agents?
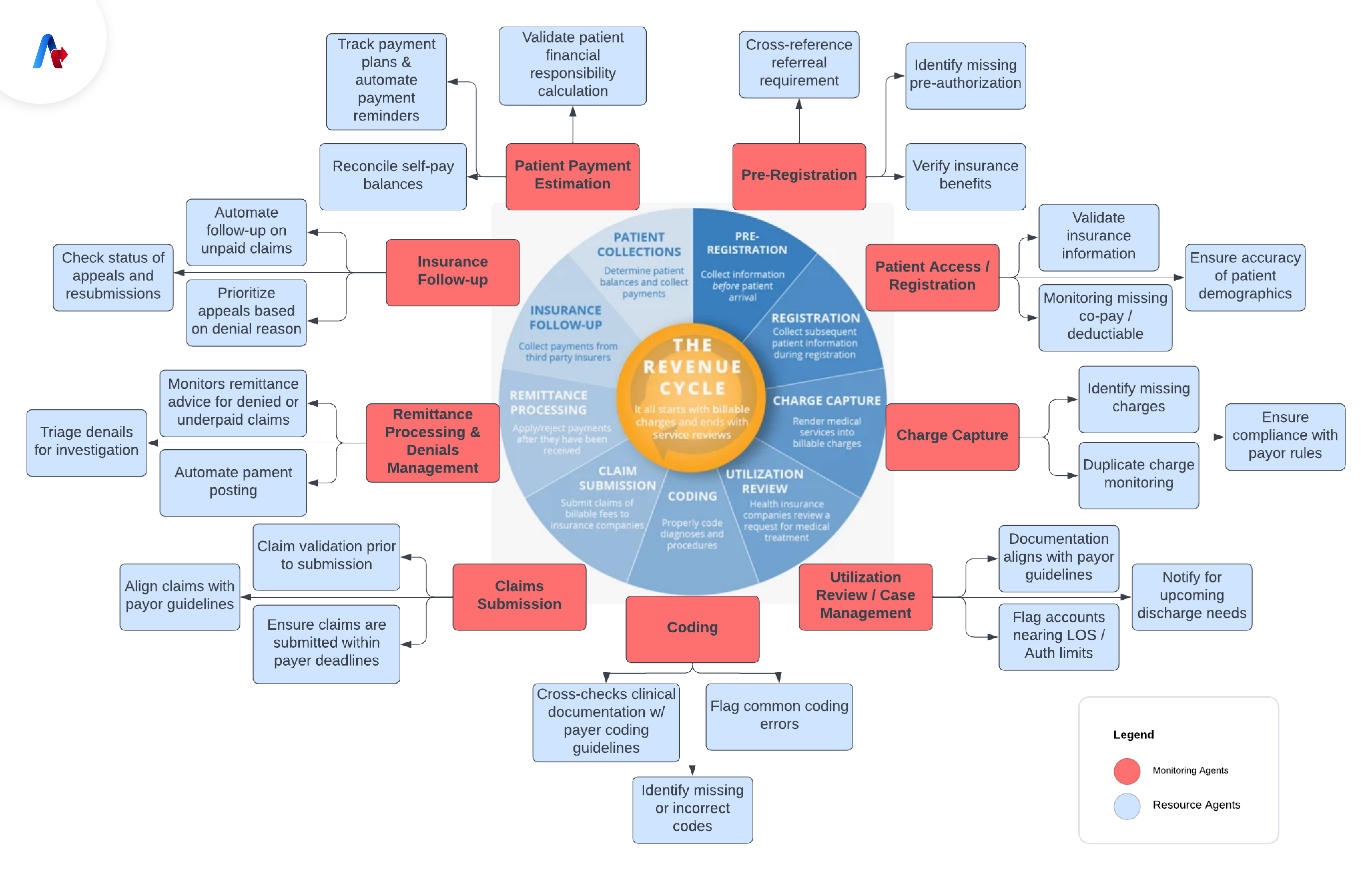
RCM is the financial process that tracks patient interactions throughout their journey—from appointment scheduling to final payment. It includes key steps like charge capture, claim submission, and payment posting.
Revenue Cycle Management automation leverages the RPA to streamline these processes. By using software ‘robots’ now upgraded to ‘agents’ to automate tasks like processing claims, posting payments, and managing denials. These agents act like humans in digital systems but perform tasks faster and more accurately on their own.
What are the Benefits of RCM Automation?
- Bots can work or operate 24/7 without fatigue, significantly reducing the time spent on tasks such as comment processing and follow-up thus increasing productivity.
- Automation reduces human error, resulting in cleaner claims and fewer rejections which indirectly improves the accuracy of the process.
- Automation acts as a cost saver by reducing manual tasks, reducing administrative costs, employees can focus on challenging and profitable activities.
- Automated revenue cycle management systems can be easily scaled to handle increased workloads without having to increase staffing levels accordingly.
How Robotic Process Automation with AI Agents Improve RCM Processes?
The use of RPA with Agentic AI in RCM brings many process improvements. The key ones are listed below.
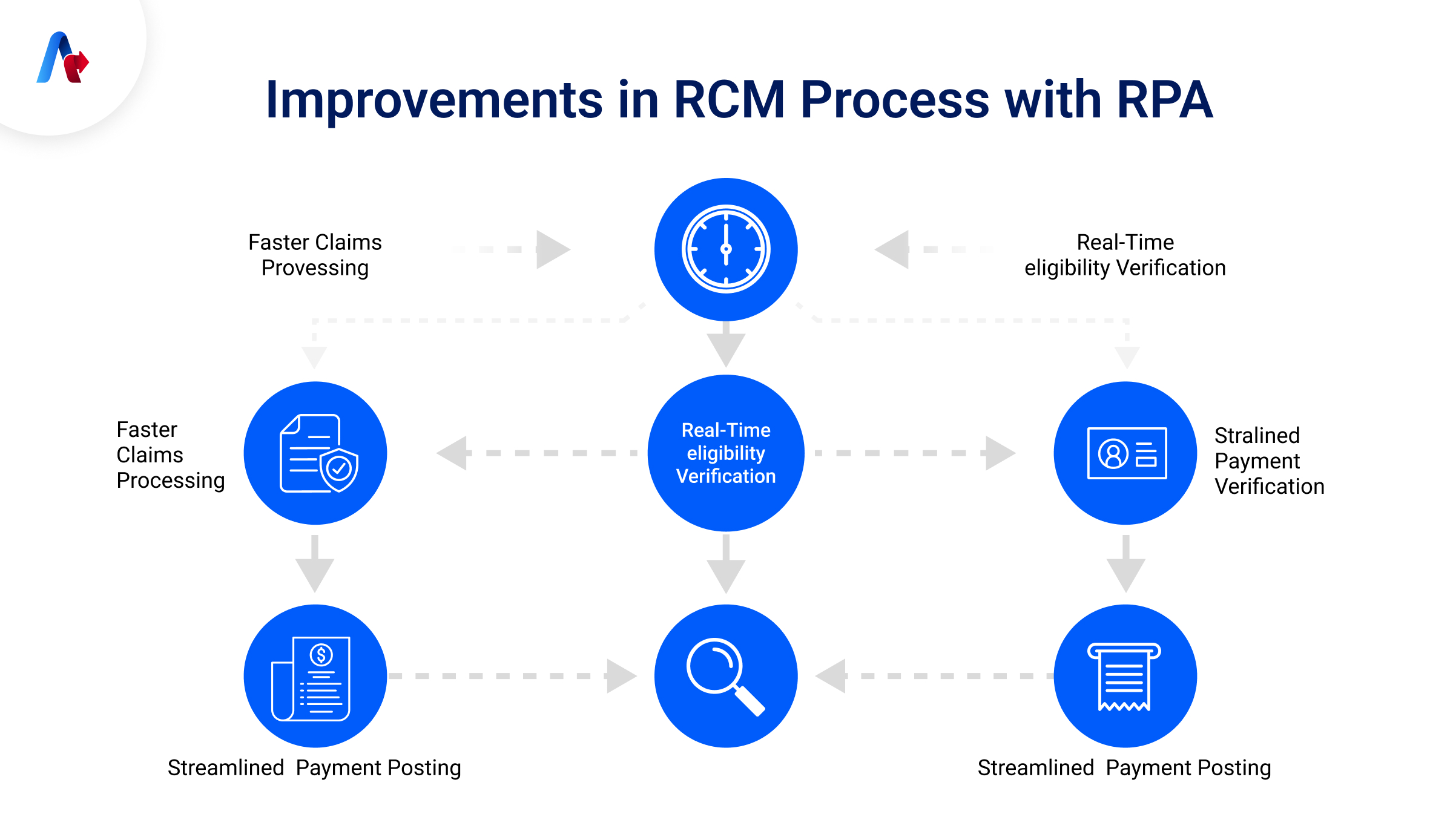
Faster Claims Processing
Automation accelerates the submission and adjudication i.e. process where one is deciding whether to accept, deny, or reject a medical claim, which results in fast reimbursement process and faster claims processing.
Real-Time Eligibility Verification
Agents can immediately/quickly view patient insurance information, ensure payment for services and reduce denials thus making sure to achieve Real-Time Eligibility Verification.
Accurate Invoice Posting
The Automated system accurately posts invoices and adjusts accounts and maintains up-to-date financial records ensuring properly maintained invoices.
Where RPA is Making an Impact in RCM?
- Claims Management: You can automate the submission of insurance documents, tracking, and management of insurance claims to reduce denials and speed up payment process.
- Denial Management: You can also automate the process of identifying, analyzing, and addressing denied claims promptly to recover revenue efficiently.
- Patient Scheduling and Registration: This is one of the basic processes in RCM which can be automated. It includes making appointment scheduling and patient intake processes streamlined to enhance patient experience and operational efficiency.
RCM Automation in Healthcare: Real-World Results
The integration of RPA with Intelligent Agents into healthcare RCM is life changing. For example, Home Care Delivered implemented RPA to automate their claims transfer process, achieving a 95% reduction in processing time and a 0% error rate on resubmitted claims. This automation allowed staff to focus on denial management, further enhancing revenue collection.
Case Studies from Healthcare Sector
- Home Care Delivered: By automating the transfer of claims from primary to secondary insurance, they saved 416 manual hours annually and achieved a 95% decrease in processing time (EnterBridge).
- Advantum Health: Robotic process automation (RPA) was introduced by Advantum Health, one of the top healthcare revenue cycle management firms, to automate tasks such as no-response claims, payment posting, and charge entry. These developments produced an impressive 292% ROI, as well as a 40% fewer FTE requirement. Medical claims submission and adjudication processes were accelerated and hence, RPA helped reimbursements faster.
- Automation also facilitated the online real-time eligibility verification of patient insurance details, which lowered claim rejection rates. Payment posting as well as recording was automated in order to keep the financial data accurate and up-to-date.
- These changes indicate that with RPA, costs can be reduced and operations improved in the healthcare industry, without compromising on the service (Advantum Health, 2025).
Scaling and Customizing RCM Automation Workflows
RPA solutions are highly scalable and customizable, allowing healthcare organizations to alter automation to their specific needs. Whether it's handling increased claim volumes or adapting to new regulatory requirements, RPA systems can be designed to meet evolving demands without significant additional investments.
Choosing the Right RCM Automation Provider
When selecting a Revenue Cycle Management automation service provider, consider the following factors:

- Experience in Healthcare: Ensure the provider has a proven track record in the healthcare industry.
- Customization Capabilities: The ability to tailor solutions to your organization's specific workflows.
- Scalability: Solutions should accommodate future growth and changes in volume.
- Support and Training: Ongoing support and comprehensive training for your staff are essential for successful implementation.
A service provider like UiPath stands out as a strong option, offering a wide range of automation solutions specifically designed for the healthcare sector. With their expertise in RPA, UiPath can help streamline RCM processes and ensure that your organization experiences smooth and efficient operations.
Factors to Consider When Implementing RCM Automation
- Process Assessment: One should evaluate current workflows to identify automation opportunities in the process.
- Stakeholder Engagement: We should involve key stakeholders to ensure buy-in and smooth transition.
- Data Security Compliance: We should ensure the automation solution complies with healthcare data security standards, such as HIPAA.
- Change Management: Finally, we should develop a strategy to manage the organizational changes that come with automation.
Partnering with Trusted and Reliable Service Providers
Collaborating with a trusted RCM automation service provider ensures a seamless integration of RPA into your revenue cycle processes. A reliable partner will offer expertise, support, and customized solutions that align with your organization's goals, ultimately leading to improved financial performance and operational efficiency.
UiPath, with its extensive experience in RPA solutions, is one such trusted partner. Their tailored services, combined with a strong support system, enable healthcare organizations to streamline their workflows and achieve measurable improvements in both operational and financial outcomes.
Role of Agentic AI in Streamlining RCM with RPA
Agentic AI plays an important role in making Revenue Cycle Management (RCM) more efficient when combined with Robotic Process Automation (RPA). With AI agents working alongside RPA, routine tasks like claims processing, eligibility checks, and payment postings are automated, but with an added advantage: AI agents help the system make smarter, data-driven decisions. They can even spot trends in claim denials and suggest ways to prevent them. This combination makes the entire process faster, more accurate, and less prone to errors, ultimately improving both the financial and operational performance of healthcare organizations.
Improve Patient Care with AI Agents-Powered RCM Automation
The adoption of RPA powered by intelligent agents in Revenue Cycle Management is improving the healthcare industry significantly by automating tedious tasks, reducing errors, and enhancing efficiency with minimal human intervention. Organizations that embrace RCM automation position themselves for improved financial health and are better equipped to focus on delivering quality patient care. Partnering with the right Agentic AI and automation partner can optimize your healthcare efforts in bringing more efficient and faster results. Talk to us today!
Got more questions?
Let’s Talk